ГисТурпМентор - симулятор гистероскопии и трансуретральной резекции
СНЯТ С ПРОИЗВОДСТВА
Характеристики
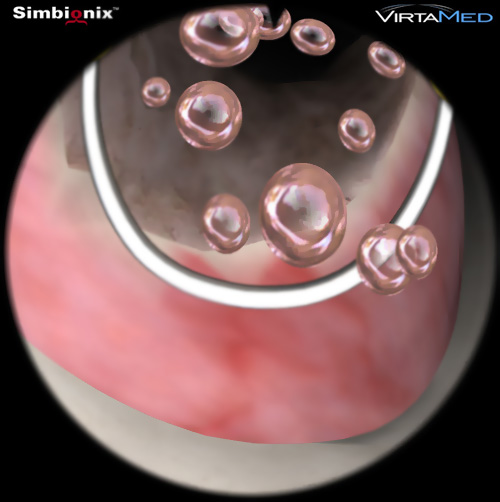
- Комбинированная платформа позволяет отрабатывать практические навыки гистероскопических процедур, гистерорезектоскопии, трансуретральной резекции простаты, трансуретральной резекции опухолей мочевого пузыря и лазерного лечения ДГПЖ
- регулируемая по высоте платформа
- два монитора для контроля симуляции и наблюдения за процессом
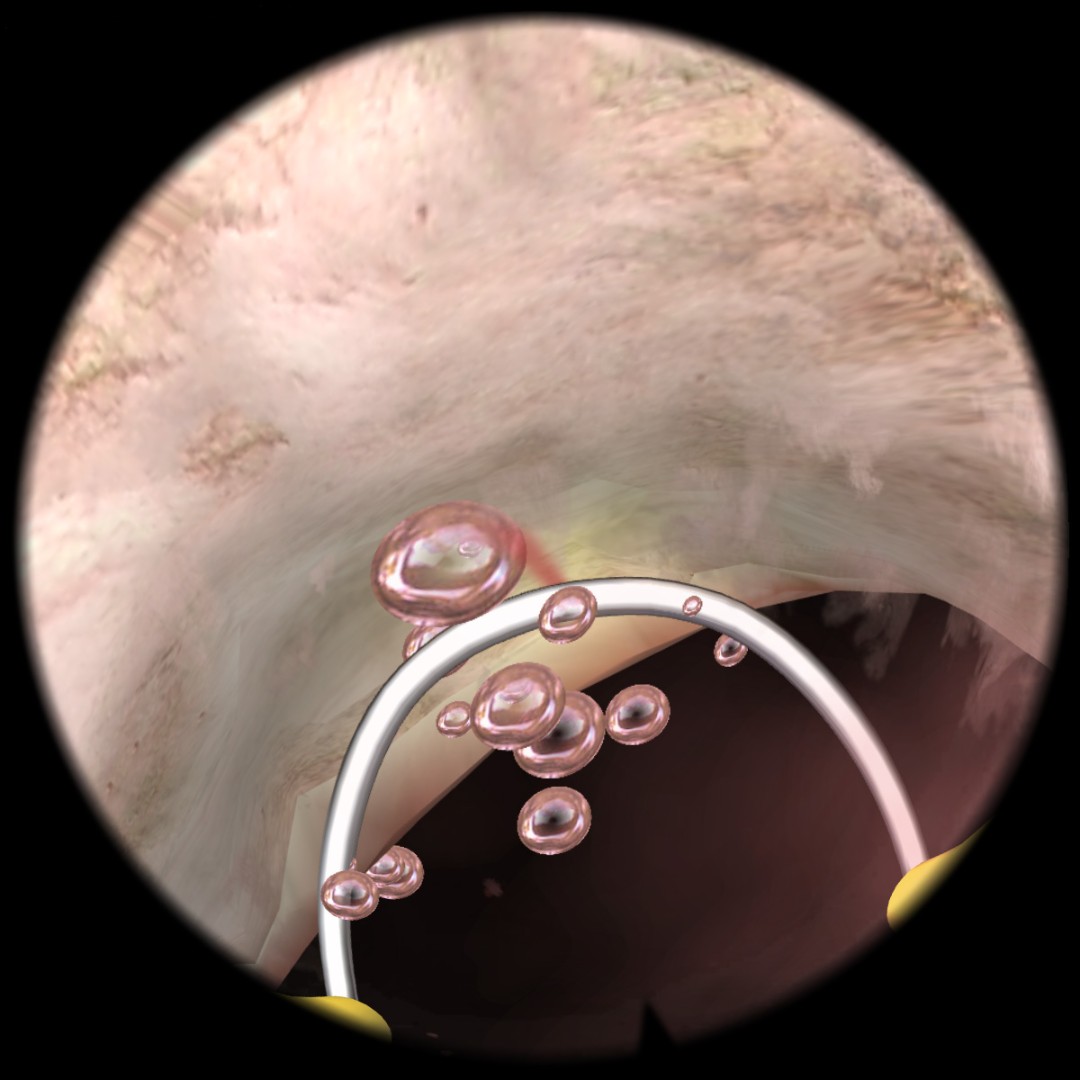
- тактильная система обратной связи с 4 степенями свободы
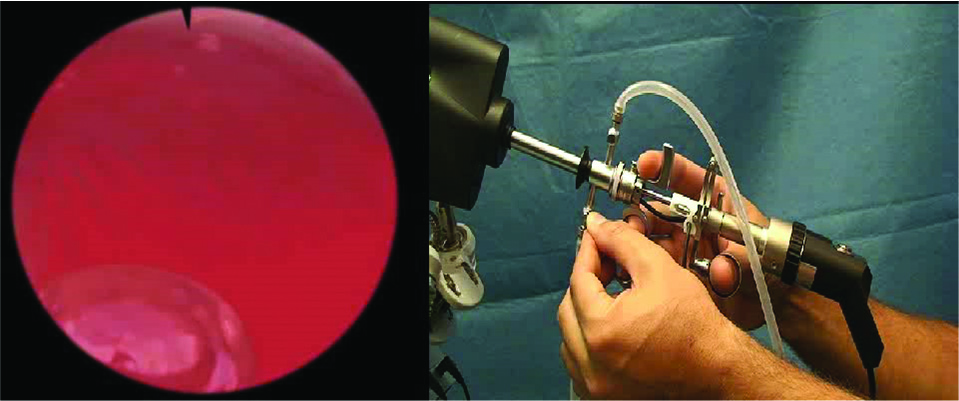
- адаптированный оригинальный резектоскоп
- полностью извлекаемый
- с впускным и выпускным клапанами для циркуляции жидкости
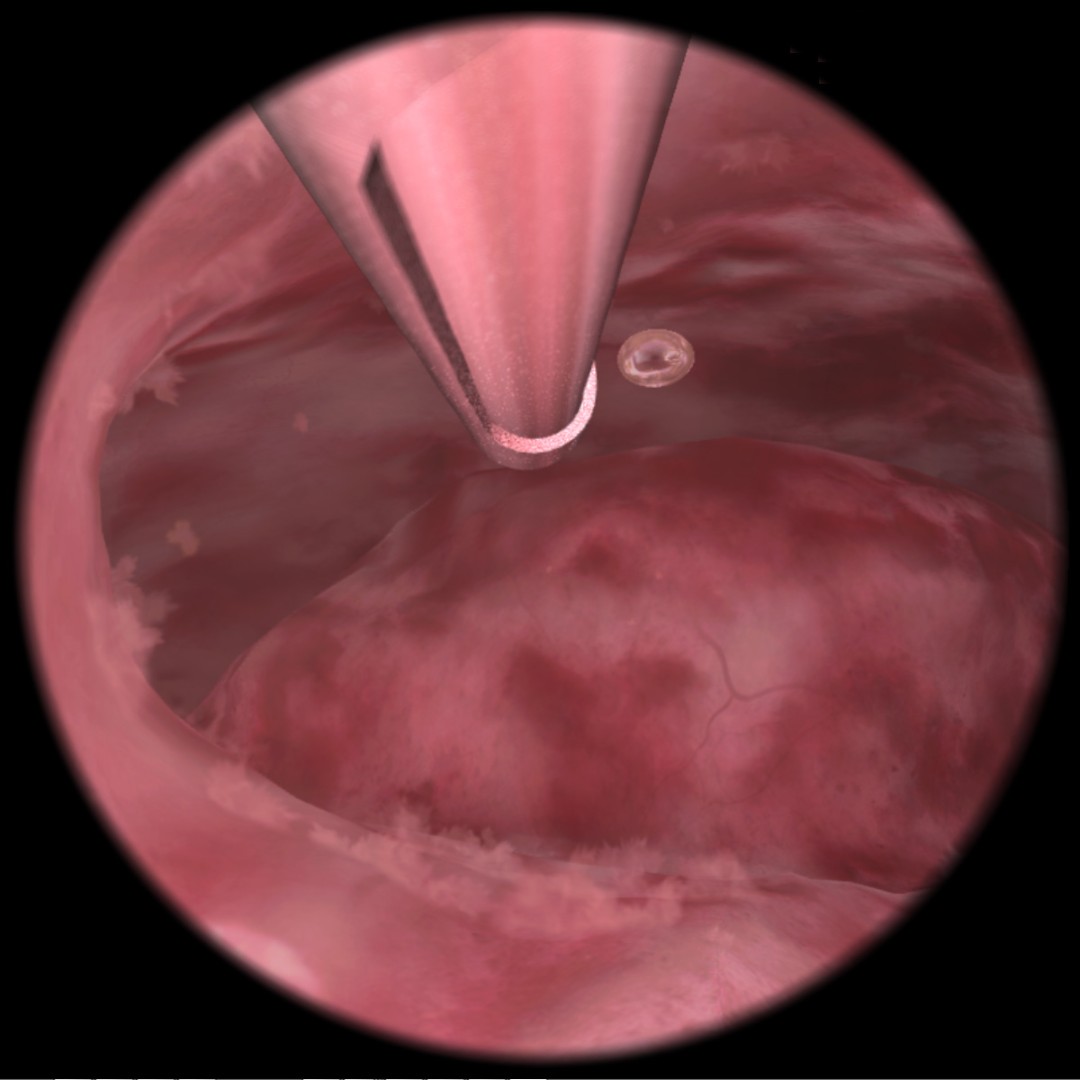
- угол обзора 0, 12 и 30 градусов
- имеет рабочие каналы для электрохирургических манипуляций
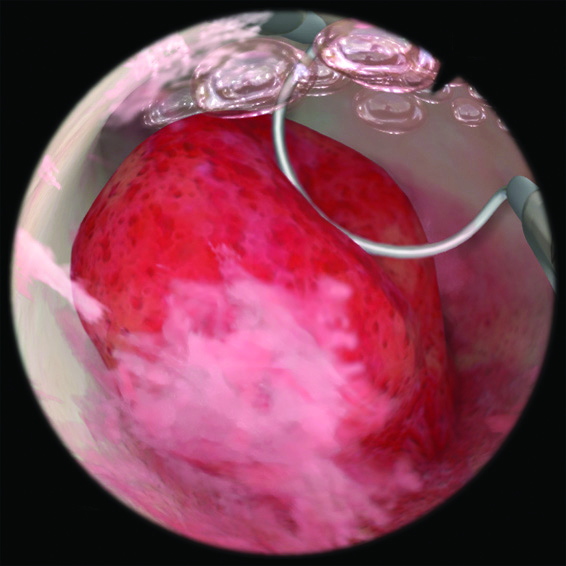
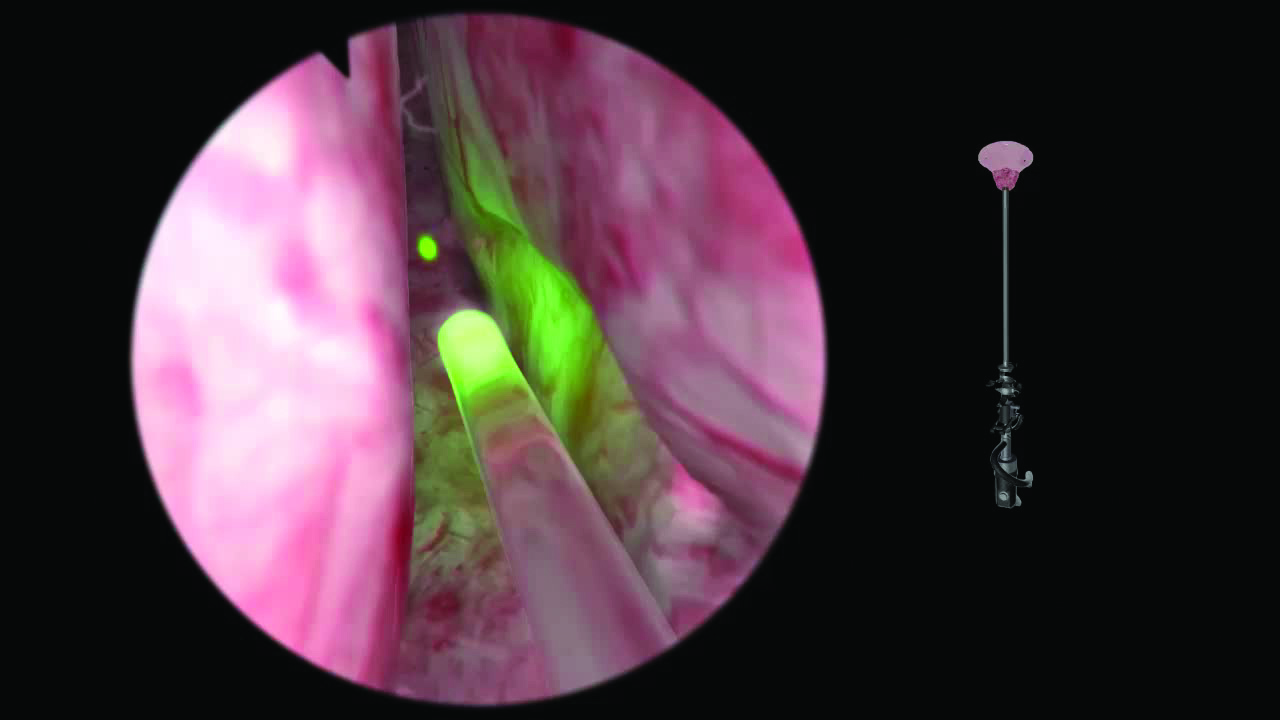
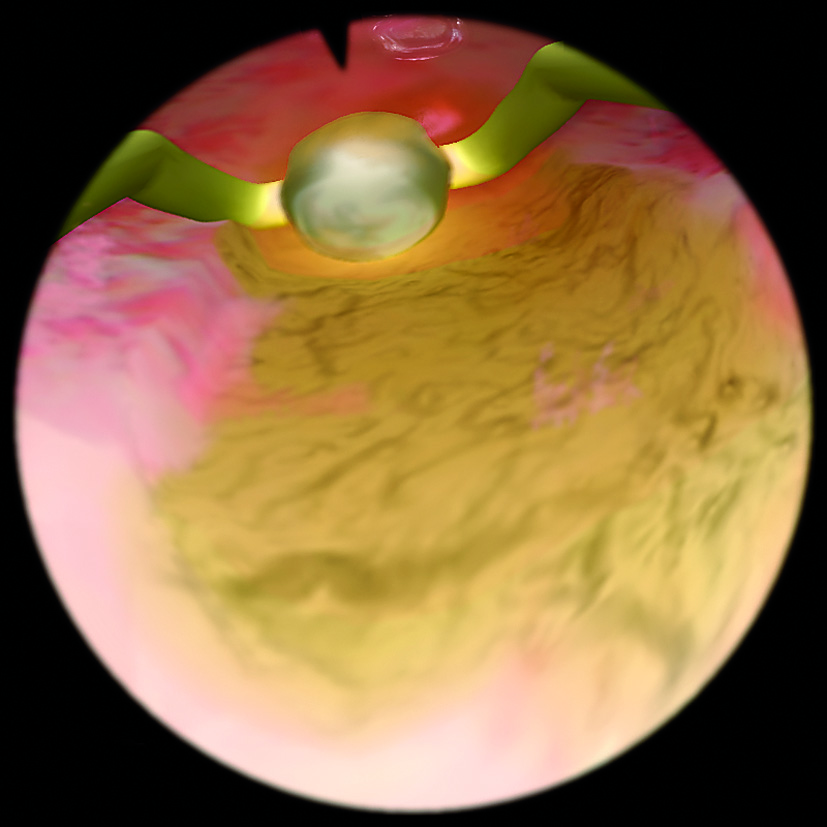
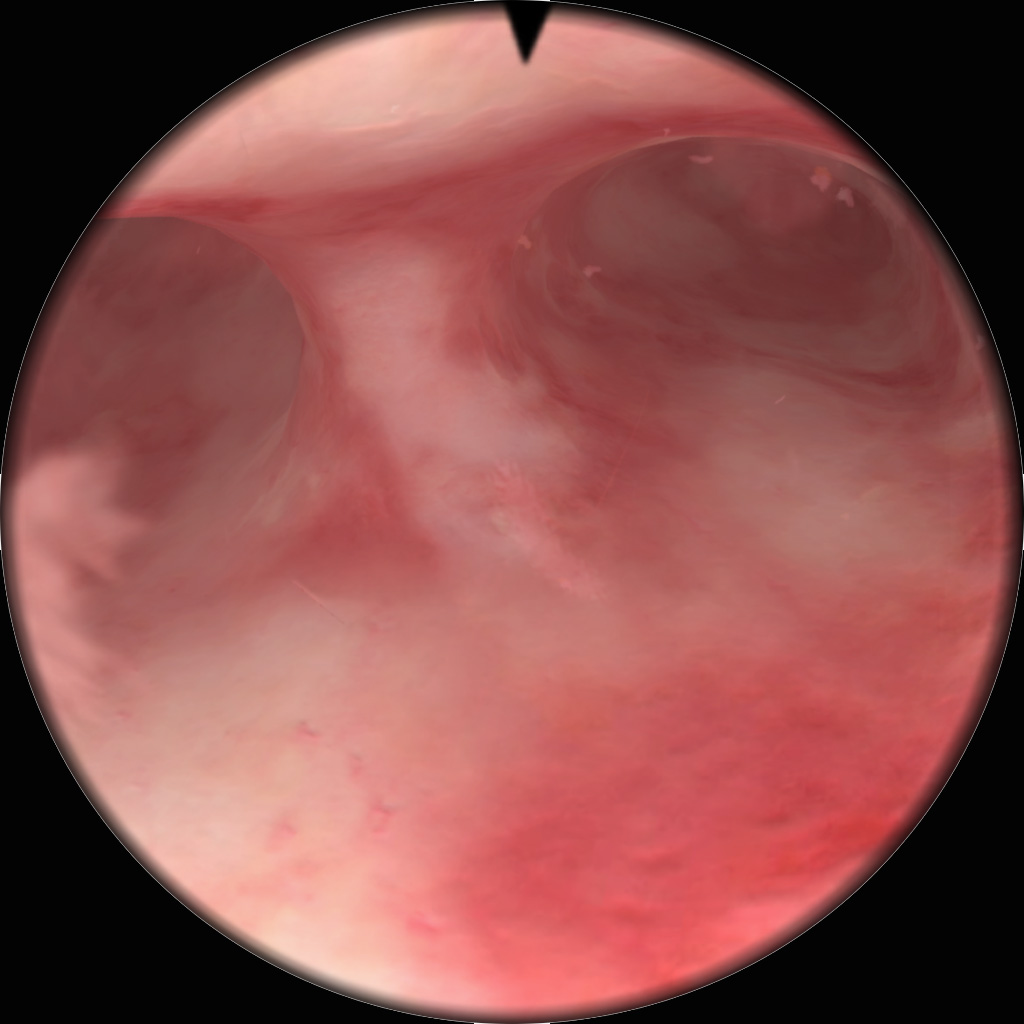
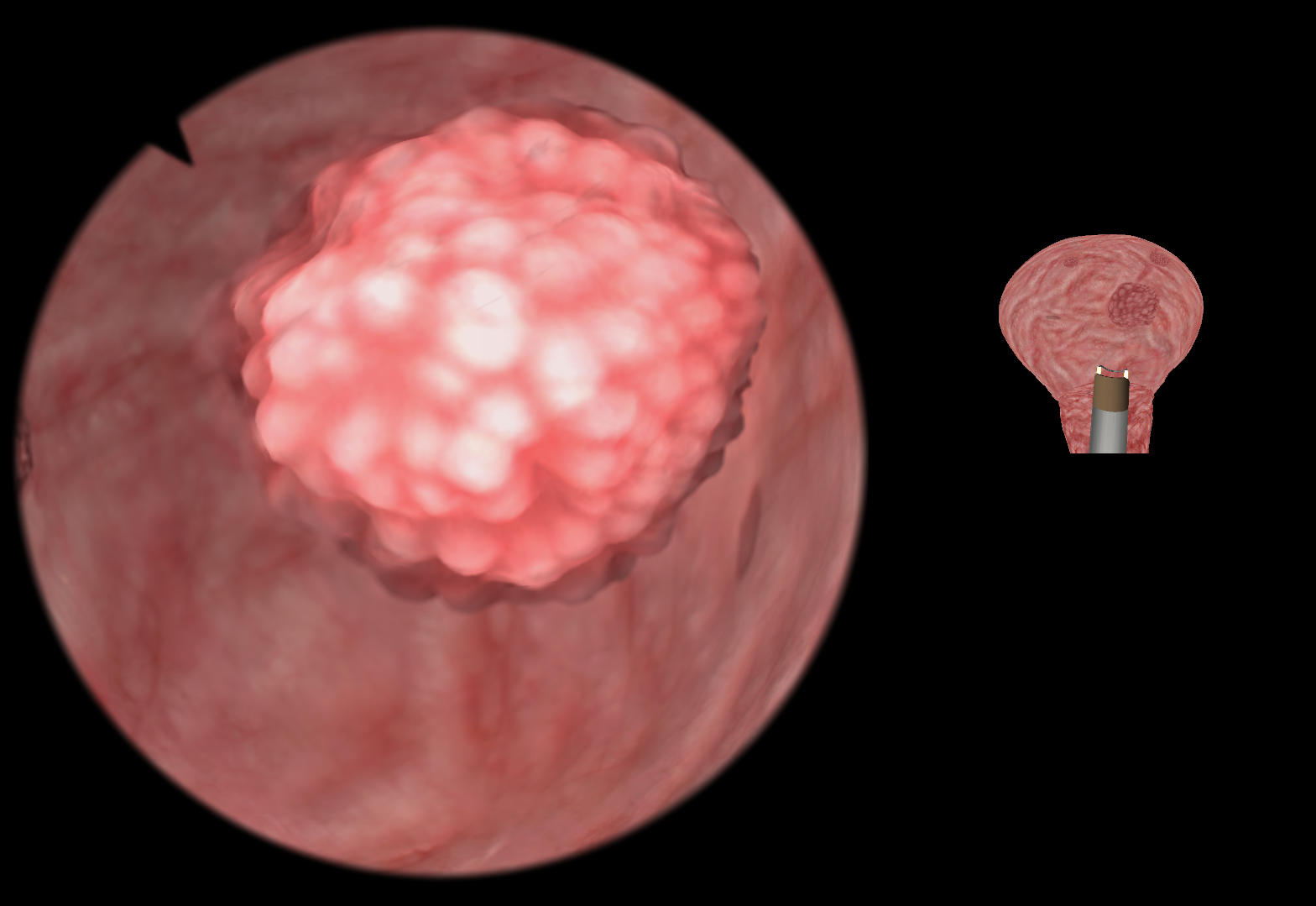
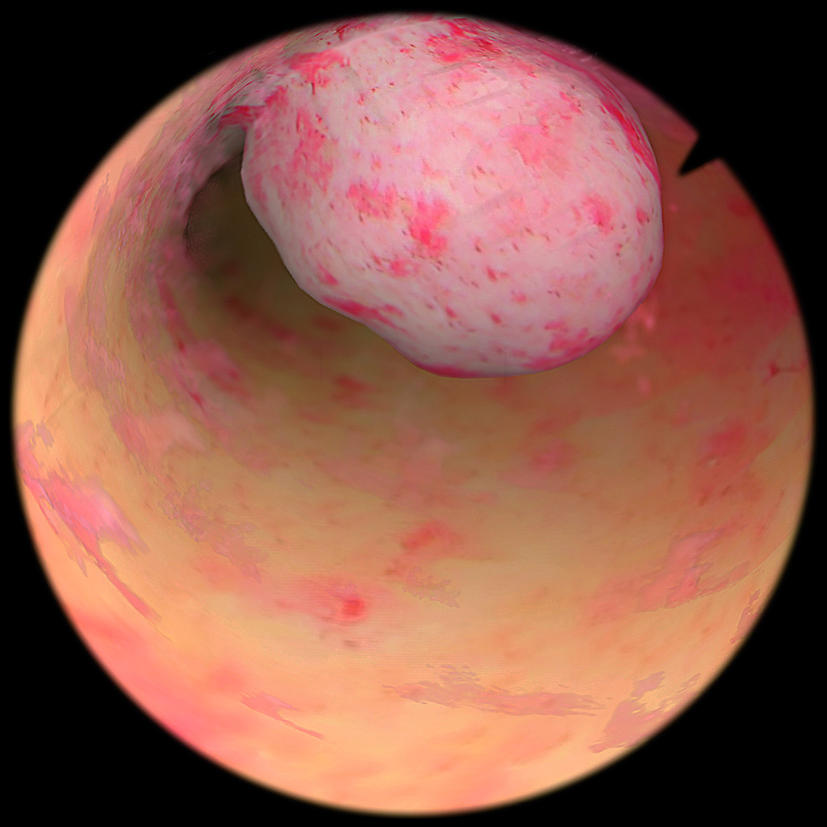
- фотореалистичное изображение
Обучающий контент
- задания с интерактивным контролем с различными уровнями сложности позволяют осваивать навыки от базовых до продвинутых
- сложные клинические сценарии с имитацией осложнений и повреждений в режиме реального времени дают возможность приобретать опыт различных подходов к выполнению процедуры
- комбинация реалистичной тактильной обратной связи, подробной анатомии, реалистичной визуализации и реальных инструментов (диагностический гистероскоп с угловой оптикой, петлевой электрод, лазерное волокно, ножницы, зажимы) и др.
- обучающий контент
- симулятор валидирован в мировых исследованиях
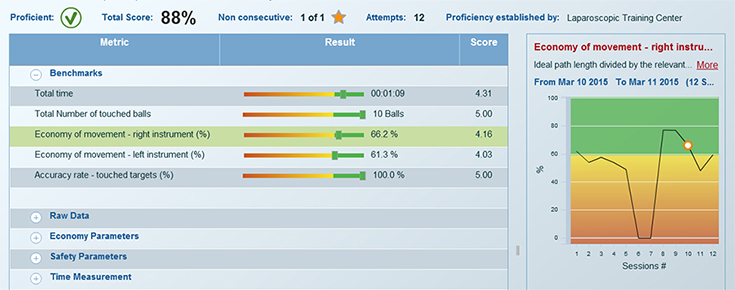
- всесторонние объективные отчеты и инструменты настройки уровня подготовленности для эффективного отслеживания прогресса в процессе обучения
МенторЛерн
Уникальная система управления учебным процессом на всех симуляторах Simbionix
Подробнее про МенторЛерн
На сегодняшний день в Российской Федерации установлено уже около 250 виртуальных симуляторов компании Simbionix, и список пользователей продолжает пополняться.
Варианты комплектации
|
SXHYST |
Симулятор ГистМентор в комплекте с модулями "Диагностическая гистероскопия", "Полипэктомия", "Миомэктомия", "Абляция эндометрия", "Расширенная резекция" |
|
SXTURP |
Симулятор ТурпМентор в комплекте с модулями "Базовые навыки ТУРП", "Полные процедуры ТУРП" |
SX-PWPU Годовое постгарантийное обслуживание симулятора
- Московский государственный медико-стоматологический университет имени А.И. Евдокимова
- Научный центр акушерства, гинекологии и перинатологии имени академика В.И.Кулакова
- Первый Московский государственный медицинский университет имени И. М. Сеченова
- Рязанский государственный медицинский университет имени академика И.П. Павлова
ТурпМентор
Visual control strategies of surgeons: a novel method of establishing the construct validity of a transurethral resection of the prostate surgical simulator.
Bright E1, Vine SJ2, Dutton T3, Wilson MR2, McGrath JS3.
1Exeter Surgical Health Services Research Unit, Royal Devon & Exeter NHS Foundation Trust, Devon, United Kingdom. Electronic address: ebright9@gmail.com.
2College of Life and Environmental Sciences, University of Exeter, St Luke’s Campus, Devon, United Kingdom.
3Exeter Surgical Health Services Research Unit, Royal Devon & Exeter NHS Foundation Trust, Devon, United Kingdom.
J Surg Educ. 2014 May-Jun;71(3):434-9.
OBJECTIVE: To examine novice and expert differences in visual control strategies while performing a virtual reality transurethral resection of the prostate (TURP) task and to determine if these differences could provide a novel method for assessing construct validity of the simulator.
SUBJECTS AND METHODS: A total of 11 novices (no TURP experience) and 7 experts (>200 TURPs) completed a virtual reality prostate resection task on the TURPsim (Simbionix USA Corp, Cleveland, OH) while wearing an eye tracker (ASL, Bedford, MA). Performance parameters and the surgeon’s visual control strategy were measured and compared between the 2 groups.
RESULTS: Experts resected a greater percentage of prostate than novices (p < 0.01) and had less active diathermy time without tissue contact (p < 0.01). Experts adopted a target-locking visual strategy, employing fewer visual fixations (p < 0.05) with longer mean fixation duration (p < 0.005). With multiple learning trials, novices’ performance improved and the adoption of a more expertlike gaze strategy was observed.
CONCLUSION: Significant differences between experts and novices in both performance and visual control strategy were observed. The study of visual control strategies may be a useful adjunct, alongside measurements of motor performance, providing a novel method of assessing the construct validity of surgical simulators.
Evaluation of the educational value of a virtual reality TURP simulator according to a curriculum-based approach.
Tjiam IM1, Berkers CH, Schout BM, Brinkman WM, Witjes JA, Scherpbier AJ, Hendrikx AJ, Koldewijn EL.
Catharina Hospital Eindhoven, Eindhoven ,Medical Centre Alkmaar (B.M.S.); EMGO Institute (B.M.S.), VU Medical Center, Alkmaar and Amsterdam; Radboud University Nijmegen Medical Centre, Nijmegen (J.A.W.); and Maastricht University, Maastricht (A.J.S.), the Netherlands.
Simul Healthc. 2014 Oct;9(5):288-94
PURPOSE: This study aimed to evaluate the place of the TURPsim (Simbionix/VirtaMed, Beit Goal, Israel) within a urologic residency training curriculum, including training needs analysis (TNA) and investigating its validity.
MATERIALS AND METHODS: Training needs analysis was conducted by an expert panel to identify procedural steps and pitfalls. Performance metrics of the simulator were compared with the TNA results. Participants were distributed according to their level of experience (completed transurethral resection of the prostate [TURP] procedures) as follows: novices (0), intermediates (1-50), and experts (>50). They followed standardized instructions and then performed 2 completeTURP procedures on the TURPsim.
RESULTS: Ten of 22 procedural steps (TNA) and 4 of 11 pitfalls were covered by the TURPsim. A total of 66 participants, 22 in each group, were included. Median general judgment (face and content) about the TURPsim was rated 7.3 (median, 7; range, 3-9). Ninety-three percent of all participants qualified the TURPsim as a useful training model. Intermediates and experts had a significant faster resection time and less blood loss compared with novices (construct) (P = 0.001). Novices needed to re-resect previous lobes, and they also resected the prostate in the incorrect order more frequently compared with intermediates and experts.
CONCLUSIONS: Training needs analysis is of paramount importance in the evaluation process of a training program. This curriculum-based approach including validity of a simulator seems valuable and may narrow the gap between skills laboratory and clinical practice. This study showed face, content, and construct validity of the TURPsim, and this simulator finds its place in the current urologic curriculum to train basic and procedural TURP skills.
The following abstract was presented at the annual meeting of the American Urological Association, May 19-23, 2012, Atlanta, Georgia
Examining the visual control strategies of experts and novices to establish the validity of a novel TURP simulator.
Thomas Dutton; Samuel Vine; John McGrath; Elizabeth Bright; Mark Wilson
INTRODUCTION AND OBJECTIVES: With increasing resource constraints and patient concern, there has been a recent interest in the use of simulators to help surgeons acquire technical skills. Surgical simulators facilitate repetitive practice and performance feedback in a risk-free environment. Previous validation of simulators has focussed on motor proficiency measures. However, studies have shown that expertise in laparoscopic skills is underpinned by an efficient visual control strategy (fixations that are long in duration and low in frequency). Using infrared eye-tracking devices, experts are seen to ‘lock’ their gaze on a target earlier and for longer, improving the accuracy of the subsequent motor skill. The aim of this study was to examine visual control measures and their utility as a novel method to assess the construct validity of a transurethral resection of prostate (TURP) virtual reality simulator (VR; Simbionix, USA Corp).
METHODS: 11 novices (no TURP experience) and 7 experts (>200 TURPS) completed the median lobe resection task on the simulator. All participants wore a gaze registration system that assessed their visual control strategy (recorded as the number of fixations per second and mean duration of fixations). The VR simulator also provided objective measures of performance (% prostate resected per minute) and safety/error (% prostatic capsule perforation and time diathermy active without tissue contact).
RESULTS: When compared to novices, experts employed a visual control strategy of fewer fixations per second (mean 1.49 vs 1.12, p < 0.05), but a longer mean fixation duration (0.43 vs 0.76, p < .005). Differences were also found in performance related measures; experts resected 59.05% of the prostate per minute whereas novices resected only 30.86% (p < .001) and experts were more precise with the diathermy than novices (0.32 vs 2.35, p < .005). However, both groups had an equal rate of prostatic capsular perforation (13.71 vs 16.91, p = 0.31). CONCLUSIONS: Significant differences have been shown in the performance of experts versus novices (proficiency and safety parameters) whilst performing a VR TURP training task. Furthermore, experts and novices displayed the expected differences in visual control strategies. This suggests that the TURP simulator is a valid tool in the replication of this common urological procedure. The study of visual control strategies may be a useful adjunct, alongside assessment of motor performance, in assessing surgeons undergoing simulation training.
This work was supported by a bilateral research_x000D_ grant from the Economic and Social Research Council, UK and the Research Grants Council, Hong Kong (RES-000-22-3016).
The following abstract was presented at the annual meeting of the American Urological Association, May 19-23, 2012, Atlanta, Georgia, USA
Learning effects using a TURP simulator: Assessing changes in visual control and performance.
Samuel Vine; Thomas Dutton; Mark Wilson; Elizabeth Bright; John McGrath
INTRODUCTION AND OBJECTIVES: Surgical simulators afford trainees the chance to practise skills in a safe environment and without the need for supervision. Although they have been proposed to shorten the learning curve for complex surgical skills, there is concern that they do not prepare trainees for the demanding conditions of the operating room. Research in skill learning (including surgical skills) has shown that experts and novices can be distinguished by differences in their visual control strategies, with experts using fewer fixations of a longer duration. The aim of this study was to assess the learning benefits of a TURP simulator by examining, not only changes in novice performance, but also changes in their visual control.
METHODS: 11 novices (no TURP experience) completed a basic training task on a virtual reality TURP simulator (Simbionix, USA Corp) whilst wearing an eye tracker to measure their visual control (number and duration of fixations). Performance measures (% prostate & % capsule resected per second) were provided by the simulator. All participants performed a baseline trial, 5 learning trials, a retention trial (to asses learning) and a tone counting trial (to mimic the multi-tasking demands of the operating theatre). All data were subjected to one-way repeated measures ANOVA and significant effects were followed up with pair-wise comparison tests.
RESULTS: Results revealed a significant improvement in performance from baseline to retention, with increases in the % of prostate resected (p < .001) and reductions in the % of capsule resected (p < .005). There was also a significant improvement in visual control from baseline to retention, with reductions in the number (p < .005) and duration of fixations (p < .05). However, there was a significant breakdown in both performance and visual control under multi tasking conditions (p’s < .005). CONCLUSIONS: After only five repetitions of a simple training task, novices became more proficient (% prostate resected) and less error full (% capsule resected), supporting the use of simulation for surgical skills training. The novices also developed more ‘expert like’ visual control, which has been shown to underpin technical skill performance. However, these changes were not robust under multi-tasking conditions, highlighting the limitations of simulated training. Future research should examine training interventions designed to ensure that visual control and motor skill performance remain robust in stressful conditions.
This work was supported by a bilateral research_x000D_ grant from the Economic and Social Research Council, UK and the Research Grants Council, Hong Kong (RES-000-22-3016).
Face validity, construct validity and training benefits of a virtual reality TURP simulator.
Bright E, Vine S, Wilson MR, Masters RS, McGrath JS.
Exeter Surgical Health Services Research Unit, Royal Devon & Exeter NHS Foundation Trust, Barrack Road, Exeter, Devon EX2 5DW, UK.
Int J Surg. 2012;10(3):163-6. Epub 2012 Feb 23.
OBJECTIVE: To assess face validity, construct validity and the training benefits of a virtual reality TURP simulator.
METHOD: 11 novices (no TURP experience) and 7 experts (>200 TURP’s) completed a virtual reality median lobe prostate resection task on the TURPsim™ (Simbionix USA Corp., Cleveland, OH). Performance indicators (percentage of prostate resected (PR), percentage of capsular resection (CR) and time diathermy loop active without tissue contact (TAWC) were recorded via the TURPsim™ and compared between novices and experts to assess construct validity. Verbal comments provided by experts following task completion were used to assess face validity. Repeated attempts of the task by the novices were analysed to assess the training benefits of the TURPsim™.
RESULTS: Experts resected a significantly greater percentage of prostate per minute (p < 0.01) and had significantly less active diathermy time without tissue contact (p < 0.01) than novices. After practice, novices were able to perform the simulation more effectively, with significant improvement in all measured parameters. Improvement in performance was noted in novices following repetitive training, as evidenced by improved TAWC scores that were not significantly different from the expert group (p = 0.18).CONCLUSIONS: This study has established face and construct validity for the TURPsim™. The potential benefit in using this tool to train novices has also been demonstrated.
ГистМентор
Using virtual-reality simulation to ensure basic competence in hysteroscopy
Savran MM, et al. Surg Endosc. 2018.
Savran MM1, Nielsen AB2, Poulsen BB3, Thorsen PB4, Konge L2,5.
Surg Endosc. 2018 Oct 17. doi: 10.1007/s00464-018-6495-3. [Epub ahead of print]
BACKGROUND: Hysteroscopy is a technically challenging procedure. Specialty curricula of obstetrics and gynaecology appraise hysteroscopy for trainees but there is no present evidence-based training program that certifies the fundamental technical skills before performance on patients. The objectives of this study were to develop and gather validity evidence for a simulation-based test that can ensure basic competence in hysteroscopy.
METHODS: We used the virtual-reality simulator HystMentor™. Six experts evaluated the feasibility and clinical relevance of the simulator modules. Six modules were selected for the test and a pilot study was carried out. Subsequently, medical students, residents, and experienced gynaecologists were enrolled for testing. Outcomes were based on generated simulator metrics. Validity evidence was explored for all five sources of evidence (content, response process, internal structure, relations to other variables, consequences of testing).
RESULTS: Inter-case reliability was high for four out of five metrics (Cronbach’s alpha ≥ 0.80). Significant differences were identified when comparing the three groups’ performances (p values < 0.05). Participants’ clinical experience was significantly correlated to their simulator test score (Pearson’s r = 0.49, p < 0.001). A single medical student managed to achieve the established pass/fail score (6.7% false positive) and three experienced gynaecologists failed the test (27.3% false negative).
CONCLUSIONS: We developed a virtual-reality simulation-based test in hysteroscopy with supporting validity evidence. The test is intended to ensure competency in a mastery learning program where trainees practise on the simulator until they are able to pass before they proceed to supervised training on patients.
Preliminary Experience with Virtual Reality Simulation vs. Animal Model for Hysteroscopic Myomectomy Training
L.R. Glazerman, S.R. Hart, M. Bajka, D. Fink, R.R. Bassaly
Glazerman LR, 1 Hart SR, 1 Bajka M, 2 Fink D, 2 Bassaly RR. 1 1Center for the Advancement of Minimally Invasive Pelvic Surgery, University of South Florida College of Medicine, Tampa, FL; 2Obstetrics and Gynecology, University Hospital of Zurich, Zurich, Switzerland
The Journal of Minimally Invasive Gynecology November 2009 (Vol. 16, Issue 6, Supplement, Page S56)
STUDY OBJECTIVE: To obtain trainees’ initial impressions of a new virtual reality hysteroscopic trainer compared to a traditional animal model for training in hysteroscopic myomectomy.
DESIGN: Attendees at a hands-on postgraduate course on operative hysteroscopy rotated through several training stations. Included in the rotation were a station using a pig bladder model for hysteroscopic myomectomy as well as a station using the HystSim (VirtaMed, Zurich, Switzerland) hysteroscopic simulator. Each participant rated both stations on realism as well as training capacity.
No significant difference was observed between the two models for realism
SETTING: Sixteen participants in a hands-on postgraduate course on operative hysteroscopy.
Patients: N/A
INTERVENTION: Immediately after a training session using either the pig bladder model or the HystSim simulator, participants were asked to rate each model on realism and training capacity using a 5-point Likert scale.
MEASUREMENTS AND MAIN RESULTS: The virtual reality trainer scored significantly higher than the pig bladder model for ‘‘variety of training cases’’ (p50.039) and ‘‘performance assessment’’ (p50.010). There was a statistically insignificant trend in favor of the virtual reality model for training capacity.
No correlation was found between age, experience, or years of practice.
CONCLUSION: The HystSim Virtual Reality hysteroscopic trainer was felt to be at least equal to the ‘‘gold standard’’ pig bladder model for training in hysteroscopic myomectomy with the additional advantages of reproducibility and measurement of results. Further studies comparing modalities and relating results to operating room performance are warranted.
Hysteroscopic placement of tubal sterilization implants: virtual reality simulator training
Pierre Panel, Michael Bajka, Arnaud Le Tohic, Alaa El Ghoneimi, Carmen Chis and Stéphane Cotin
Service de Gynécologie-Obstétrique, Centre Hospitalier de Versailles, Hôpital André Mignot, 177 avenue de Versailles, 78157, Le Chesnay, France
Surgical Endoscopy 2012, DOI: 10.1007/s00464-011-2139-6
STUDY OBJECTIVE: To assess face and construct validity of a new virtual reality (VR) training simulator for hysteroscopic placement of tubal sterilization implants.
DESIGN: Nonrandomized, controlled trial comparing responses and performance of novices and experts on the simulator. Classification: Canadian task force II-1.
SETTING: Forty-six gynecologists were personally invited or recruited at the 33rd Conference of the French National College of Gynecologists and Obstetricians (CNGOF) from December 9 to 12, 2009, grouped as 20 experts and 26 novices. They all performed the defined sequence of virtual procedures on the simulator (case 1 for familiarization, case 4 for study assessment) and finally completed the study questionnaire.
MEASUREMENTS AND MAIN RESULTS: Responses to realism, educational potential, and general opinion were excellent, proving face validity. Significant differences between novices and experts were assessed for 7 of the 15 metrics analyzed, proving construct validity.
CONCLUSIONS: We established face and construct validity for EssureSim™, an educational VR simulator for hysteroscopic tubal sterilization implant placement. The next steps are to investigate convergent and predictive validity to affirm the real capacity of transferring the skills learned on the training simulator to the patient in the operating room.
The following abstract was presented at the Annual Congress of the European Society for Gynaecological Endoscopy (ESGE), September 21-24, 2011 London, UK
Face & Construct Validity of a Virtual Reality Simulator for Hysteroscopy Essure Sterilization
J.A. Janse1, S. Veersema1, F. Broekmans, H.W.R.2 Schreuder2
1 St. Antonius Hospital Nieuwegein, Netherlands
2University Medical Centre Utrech, Netherlands
INTRODUCTION: The face and construct validity of a new virtual reality simulator for the hysteroscopy Essure sterilization method is established by determining the extent of realism of the simulation to the actual task and by analysis of the performance of participants with varying hysteroscopy experience.
OBJECTIVE: The aim of this study is to determine face and construct validity of the EssureSim™, a new virtual reality simulator for the Essure sterilization method.
METHODS: Residents and gynecologists (N=63) were recruited for voluntary participation. Three groups were made based on hysteroscopy experience: novices (N=10), intermediates (N=43) and experts (N=10). Participants completed three exercises. The second and third exercises were used for analysis. Parameters ‘time’, ‘path length’, ‘patient comfort’, ‘successful placement’, ‘trauma’ and ‘distension medium’ were compared between groups to determine construct validity. Afterwards, participants filled out a questionnaire addressing hysteroscopy experience and the simulator. By analysis of the questionnaire face validity was determined.
RESULTS: The experts performed both exercises significantly faster than the novice group (p<.05). The novices had a longer path length in the first exercise in comparison to the intermediate and expert group (p<.05). Analysis of the other parameters did not show any significant results between groups. In the questionnaire realism and training capacity of the EssureSim™ were both scored with a median of 4 points on a 5-point Likert scale. Of all participants, 96.8% indicated the EssureSim™ as a useful preparation for real-time Essure placement.
CONCLUSION: Face and construct validity was established of the EssureSim™ and this simulator is considered to be a useful training method for different levels of expertise. Virtual reality simulation could offer a significant contribution to the training of hysteroscopy skills.
Establishing Construct Validity of a Virtual-Reality Training Simulator for Hysteroscopy Via a Multimetric Scoring System
Michael Bajka Æ Stefan Tuchschmid Æ Daniel Fink Æ Ga´bor Sze´kely Æ Matthias Harders
Clinic of Gynaecology, Dept. OB/GYN, University Hospital Zurich, 8091, Zurich, Switzerland
Surg Endosc. 2009 June 24.
BACKGROUND: The aims of this study are to determine construct validity for the HystSim virtual-reality (VR) training simulator for hysteroscopy via a new multimetric scoring system (MMSS) and to explore learning curves for both novices and experienced surgeons.
METHODS: Fifteen relevant metrics had been identified for diagnostic hysteroscopy by means of hierarchical task decomposition. They were grouped into four modules
(visualization, ergonomics, safety, and fluid handling) and individually weighted, building the MMSS for this study. In a first step, 24 novice medical students and 12 experienced gynecologists went through a self-paced teaching tutorial, in which all participants received clearly stated goals and instructions on how to carry out hysteroscopic procedures properly for this study. All subjects performed five repeated trials on two different exercises on HystSim (exploration and diagnosis exercises). After each trial the results were presented to the participants in the form of an automated objective feedback report (AOFR). Construct validity for the MMSS and learning curves were investigated by comparing the performance between novices and experienced surgeons and in between the repeated trials. To study the effect of repeated practice, 23 of the novices returned 2 weeks later for a second training session.
RESULTS: Comparing novices with the experienced group,the ergonomics and fluid handling modules resulted in construct validity, while the visualization module did not,
and for the safety module the experienced group even scored significantly lower than novices in both exercises. The overall score showed only construct validity when the
safety module was excluded. Concerning learning curves, all subjects improved significantly during the training on HystSim, with clear indication that the second training session was beneficial for novice surgeons.
CONCLUSIONS: Construct validity for HystSim has been established for different modules of VR metrics on a new MMSS developed for diagnostic hysteroscopy. Careful
refinement and further testing of metrics and scores is required before using them as assessment tools for operative skills.
Evaluation of a New Virtual-Reality Training Simulator for Hysteroscopy
Bajka M, Tuchschmid S, Streich M, Fink D, Székely G, Harders M.
Clinic of Gynaecology, Dept. OB/GYN, University Hospital Zurich, 8091, Zurich, Switzerland
Surg Endosc. 2008 Apr 24.
BACKGROUND: To determine realism and training capacity of HystSim, a new virtual-reality simulator for the training of hysteroscopic interventions.
METHODS: Sixty-two gynaecological surgeons with various levels of expertise were interviewed at the 13(th) Practical Course in Gynaecologic Endoscopy in Davos, Switzerland. All participants received a 20-min hands-on training on the simulator and filled out a four-page questionnaire. Twenty-three questions with respect to the realism of the simulation and the training capacity were answered on a seven-point Likert scale along with 11 agree-disagree statements concerning the HystSim training in general.
RESULTS: Twenty-six participants had performed more than 50 hysteroscopies (“experts”) and 36 equal to or fewer than 50 (“novices”). Four of 60 (6.6%) responding participants judged the overall impression as “7 – absolutely realistic”, 40 (66.6%) as “6 – realistic”, and 16 (26.6%) as “5 – somewhat realistic”. Novices (6.48; 95% confidence interval [CI] 6.28-6.7) rated the overall training capacity significantly higher than experts (6.08; 95% CI 5.85-6.3), however, high-grade acceptance was found in both groups. In response to the statements, 95.2% believe that HystSim allows procedural training of diagnostic and therapeutic hysteroscopy, and 85.5% suggest that HystSim training should be offered to all novices before performing surgery on real patients.
CONCLUSION: Face validity has been established for a new hysteroscopic surgery simulator. Potential trainees and trainers assess it to be a realistic and useful tool for the training of hysteroscopy. Further systematic validation studies are needed to clarify how this system can be optimally integrated into the gynaecological curriculum.
















.jpg)











.jpg)